Pulmonary Function Studies
Lung Volumes

While spirometry does provide the bulk of the data for a pulmonary assessment, there are frequent occasions where the data indicates mixed restrictive and obstructive disease which can only be clarified with the measurement of lung volumes. The technique for the assessment of lung volumes shares a similar origin story to spirometry, in that the concept was recognized in the last 1800's, but it was not practical for widespread application until the 1950's. I recall a story from the program director in my pulmonary fellowship, how his program cobbled together a box for the measurement of lung volumes using a repurposed hatch from a submarine.
There are two techniques for the measurement of lung volumes; body plethysmography and nitrogen wash-out. The later is an older and less accurate technique that shares its conceptual physiology with our final parameter of complete pulmonary function studies (Diffusion Capacity). While the patient is performing tidal volume breathing, the technician swaps the patient to a closed system where the patient inhales 100% oxygen and measures the change in the nitrogen consentration. Depending on the degree of low ventilation/perfusion units, a new concentration of nitrogen will be extablished equal to the added volume of the thoracic space. This technique requires somewhere between 3-4 minutes in em healthy em subject and may take longer than 15 minutes in individuals with COPD. Even with this added time, the study often underestimates the degree of air trapping. As a result most labs that perform the measurement of lung volumes has transitioned to the faster and more accurate body plethysmography.
Both techniques for the calculation of lung volumes measure the FRC. Why choose this parameter rather than Total Lung Capacity (TLC) or Residual Volume (RV)?
In body plethysmography, the patient is placed in a sealed compartment and breaths through a mouth piece. At FRC, a shutter occuludes the mouth piece and the patient is instructed to pant for several breaths. Based on Boyles Law the change in pressure within the closed chamber is related to the additional volume, hence the calculation of FRC. In addition by looking at the change in mouth pressure you can also caluclate airway resistence.
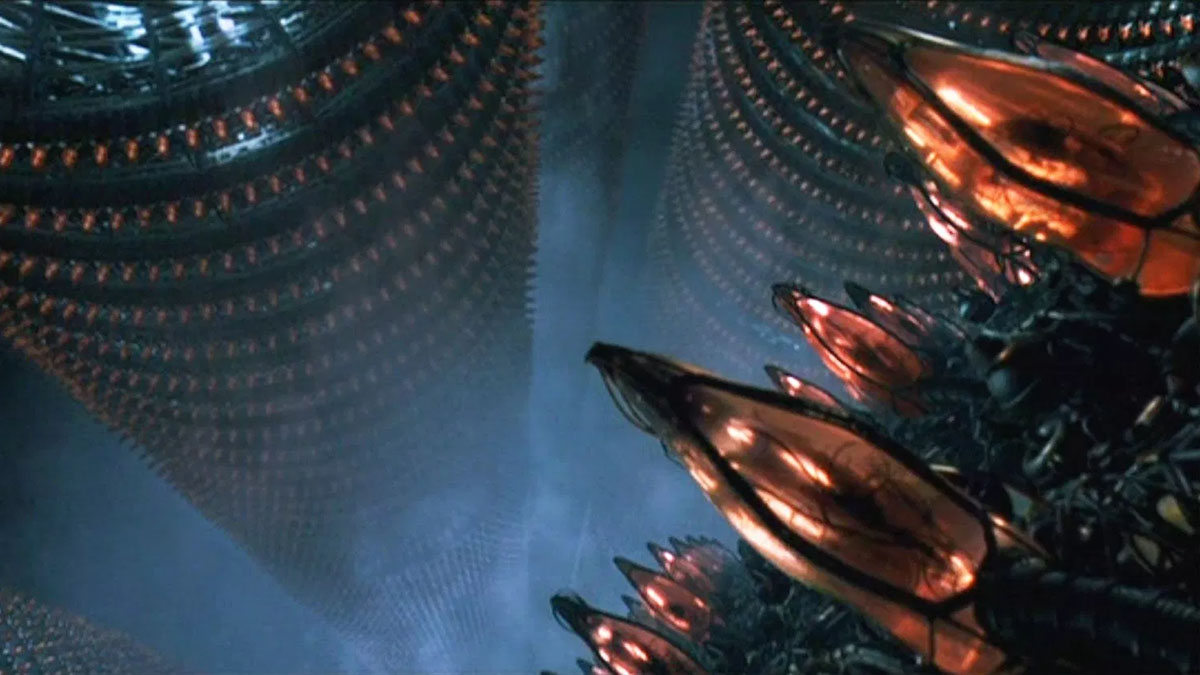
Is it me or doesn't this remind you of......
Having undergone full pulmonary function studies at several points in my career, I can say that the process of performing lung volume calculation was the most stressful part of the exam and I have healthy lungs.
Based on your knowledge of body plethysmography what would you anticipate may be issues with the performance of this study?
The end result of lung volume measurement is the calculation of FRC and utilizing the data from a vital capacity maneuver you can calculate TLC and RV. Once parameter you may see in evaluating a PFT report is that of Slow Vital Capacity (SVC). In persons with airway obstruction, the increase in intrathoracic pressure with a FVC maneuver will increase the dynamic collapse of the airway and lead to cessation of airflow at less than residual volume. With the SVC maneuver the patient exhales in a much slower fashion and the resultant measurement show be a more accurate measurement of RV. Some simple spirometers allow the performance of a SVC maneuver and when the SVC is greater than the FVC it suggests the presence of air trapping. Calculations from FRC:
| Calculated Value | Formula |
|---|---|
| Total Lung Capacity (TLC) | FRC + Inspiratory Capacity (IC) |
| Residual Volume (RV) | TLC - FVC (SVC) |
| Expiratory Reserve Volume (ERV) | FRC - RV |
| PFT Pathology | TLC | RV | RV/TLC | ERV |
|---|---|---|---|---|
| Restrictive Disease | low | low | normal | normal |
| Air Trapping | normal | elevated | elevated | low |
| Restrictive Disorder with Air Trapping | low | normal to minimal elevated | elevated | low |
| Obesity or Diaphragm Weakness | normal | normal to mildly elevated | midly elevated | low |
TLC is primarily used as a confirmation of restriction, not to determine its severity (see FVC parameters). Air trapping can be classified based on the elevation of the RV and to a lesser certain degree with RV/TLC ratio:
| Imapirment | RV or RV/TLC | Z-score |
|---|---|---|
| Normal | 80-125% predicted | Less 1.65 |
| Mild Air Trapping | 125-150% predicted | 1.64 - 2.5 |
| Moderate Air Trapping | 150-180% predicted | 2.5 - 3.5 |
| Moderately Severe Air Trapping | 180-200% predicted | 3.5 - 4.5 |
| Severe Air Trapping | > 200% predicted | > 4.5 |
It has been observed that RV tends to correlate more closely with the degree of dyspnea than the FEV1 in patients with obstructive lung disease. A caveat I mentioned from my personal experience with the performance of body plethysmography is challenges of this procedure. As a result when compared to spirometry, even well coached FRC determination can have a day to day variability of 15%. So the use of these values for the assessment of clinical response or deterioration must be more measured and conservative.