Pulmonary Function Studies
Post Bronchodilator Testing
Thus far all the parameters we have measures in the assessment of lung function are steady state parameters. Reassessing spirometry after the administration of inhaled bronchodilators is often a valuable dynamic assessment.
Since the advent of modern spirometry in the 50s and 60s there has been an interest in the acute effects of bronchodilator administration on lung function. Despite 60+ years of interest, there is still a heated debate about the implications and determination of an bronchodilaotr response.
The first is what agent should be used and how should it be administered. Most pulmonary function labs will use either inhaled albuterol (4 puffs) or an albuterol nebulizer (2.5mg) wait 15 minutes and then perform repeat spirometry. It has been argued that a short acting mucarinic agent such as ipratropium should also be used to acheive maximal dilation.
A related controversy is what medications should be withheld prior to bronchodilator testing and for how long. It is generally accepted that short acting agents should be held for 4-6 hours, but there is no clear standard for long acting agents.
The next controversy is what constitutes a positive response. For many decades, the criteria was based on the percent improvement comparing the pre/post bronchodilator values using the formula (post value - prevalue)/prevalue * 100. A clinically signficant improvement was considered at least a 12% difference between the two values. A statical fluke of low spirometric values is that the absolute improvement to acheive a 12% change may be "clinically" insignificant. Conversely in patient's with well preserved lung function we would need a far larger response to meet the 12% threshold. Therefore a secondary criteria was added of a 200ml absolute improvement.
If was suggested by the European Respiratory Society, that a more valid measurement would be to compare the percent predicted for the pre and post value and if the absolute difference between the two percent predicted values was at least 10% this would be considered a clinically significant response. This criteria has not been widely adopted in the United States.
The Global Lung Initiative (GLI) has suggested a third criteria of an absolute improvement greater than 10% of the predicted normal for the parameter.
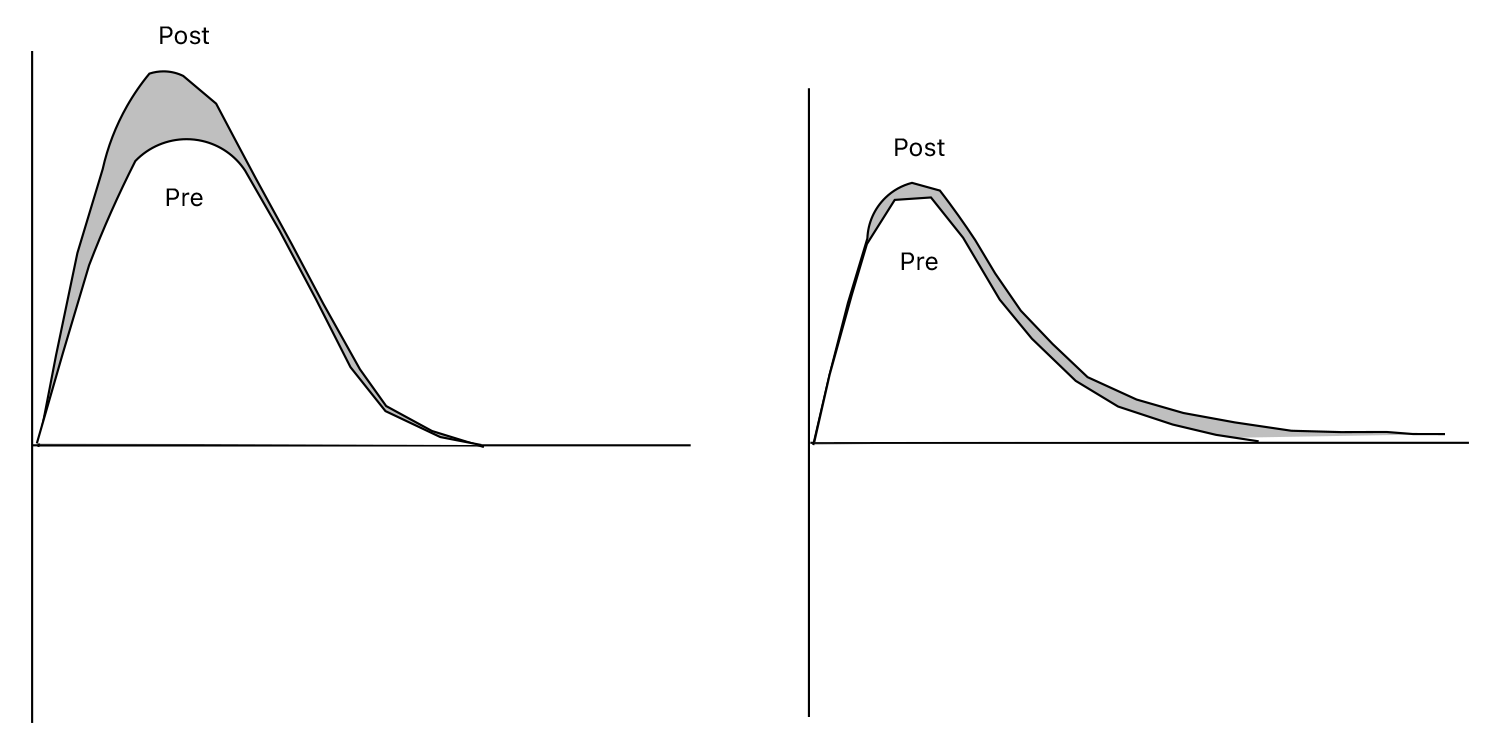
An additional aspect is that one may see in only a portion of the spirometry, such as either the FEV1 or the FVC.
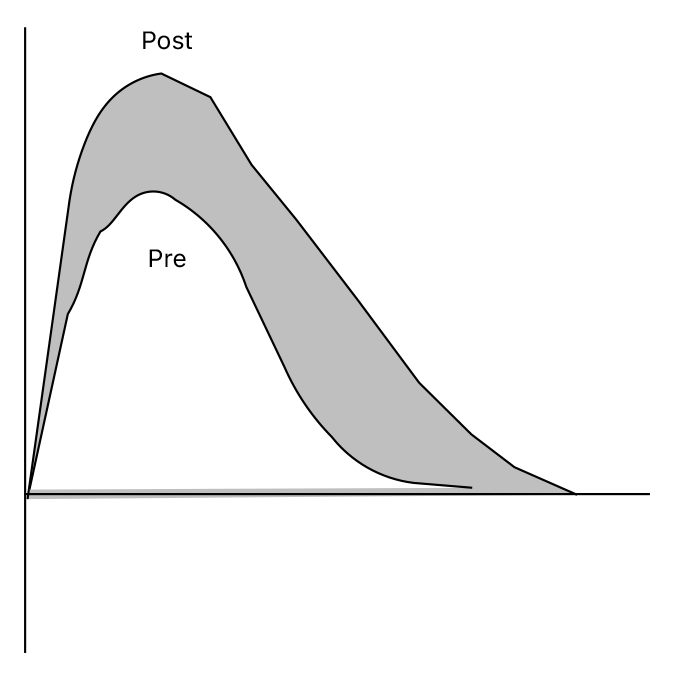
Because this determination often falls into a gray zone, I include a visual assessment of the Flow-Volume and Volume-Time loops into my evaluation process. If there is airbetween the two loops this is secondary reinforcement of a clinically revalent response.
The final controversy resolves around the clincal implications of a bronchodilator response. Historically is has been viewed as an indicator of airway reactivity and the presence of asthma. Consequently a patient that would benefit from an inhaled steroid.
But to borrow from one of the more quotable movies "The Princess Bride" :
"I dont think that means, what you think it means"
I have attended discussions were it has been suggested to use a 'steroid trial' due determine if the patient has reversibility. In this setting a patient is given a modest dose of oral prednisone for 1 month and then has repeat spirometry to see if there is an improvement.